Inflammation: A novel target of current therapies for hepatic encephalopathy in liver cirrhosis

Improvement of the Modeling and Diagnosis of Hepatic Encephalopathy in Rats
20.09.2019
Intestinal-borne dermatoses significantly improved by oral application of Escherichia coli Nissle 1917
20.09.2019
Authors: Ming Luo, Jian-Yang Guo, Wu-Kui Cao.
Abstract
Hepatic encephalopathy (HE) is a severe neuropsychiatric syndrome that most commonly occurs in decompensated liver cirrhosis and incorporates a spectrum of manifestations that ranges from mild cognitive impairment to coma. Although the etiology of HE is not completely understood, it is believed that multiple underlying mechanisms are involved in the pathogenesis of HE, and one of the main factors is thought to be ammonia; however, the ammonia hypothesis in the pathogenesis of HE is incomplete. Recently, it has been increasingly demonstrated that inflammation, including systemic inflammation, neuroinflammation and endotoxemia, acts in concert with ammonia in the pathogenesis of HE in cirrhotic patients. Meanwhile, a good number of studies have found that current therapies for HE, such as lactulose, rifaximin, probiotics and the molecular adsorbent recirculating system, could inhibit different types of inflammation, thereby improving the neuropsychiatric manifestations and preventing the progression of HE in cirrhotic patients. The antiinflammatory effects of these current therapies provide a novel therapeutic approach for cirrhotic patients with HE. The purpose of this review is to describe the inflammatory mechanisms behind the etiology of HE in cirrhosis and discuss the current therapies that target the inflammatory pathogenesis of HE.
INTRODUCTION
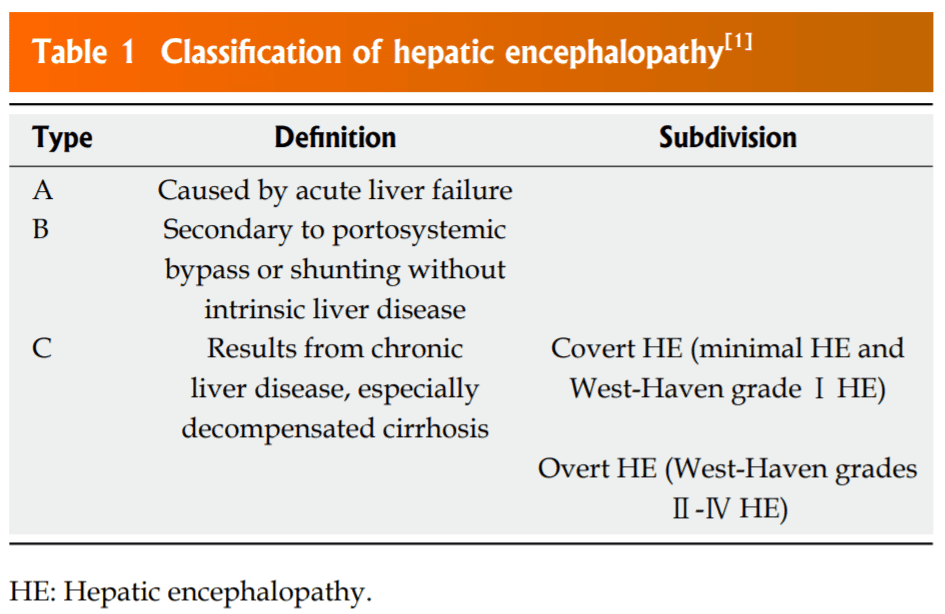
Hepatic encephalopathy (HE) is a morbid neuropsychiatric complication resulting from decompensated liver disease or portosystemic shunting and is characterized by disturbances of both cognitive and motor functions, ranging from subtle psychometric abnormalities to coma[1]. According to the updated guideline, HE is classified into three different types: A, B and C (Table 1)[1]. Subsequently, based on the severity of the clinical manifestations, type C HE is subdivided into covert HE (including minimal HE and West-Haven gradeⅠHE) and overt HE (WestHaven grades Ⅱ-Ⅳ HE)[1]. Cirrhotic patients with overt HE present a series of severe neuropsychiatric manifestations, such as asterixis, dyspraxia, and even progressing to stupor and coma. In contrast, minimal HE exhibits trivial cognitive deficits that are only detected using psychometric or neurophysiological tests without the obvious manifestations of overt HE[2]. Minimal HE impairs cognitive functions and health-related quality of life in cirrhotic patients and is considered an important predictive factor for the development of overt HE[3,4].
In spite of several decades of investigation, the exact mechanisms responsible for the pathogenesis of HE still have not been fully elucidated. Ammonia is universally regarded as the major precipitating factor in the pathogenesis of HE, and the vast majority of the current therapies for HE are centered on reducing the production and absorption of ammonia; however, several studies have suggested that the concentration of ammonia can be elevated in the absence of symptoms of HE, and the ammonia concentration is not always consistent with the severity of HE in cirrhotic patients[5-7]. Furthermore, approximately 20% of patients with chronic liver failure and HE have been found to be non-responsive to lactulose treatment, and it has been demonstrated that non-absorbable disaccharides do not reduce the mortality of cirrhotic patients with HE[8,9]. Apart from hyperammonemia, various other pathogenic mechanisms, such as the γ-aminobutyric acid (GABA) theory, the benzodiazepine theory, the manganese theory and the theory of oxidative/nitrosative stress, have been implicated in the development of HE[1]. Currently, it is believed that HE is a result of multiple pathophysiologic mechanisms that induce the functional impairment of the central nervous system.
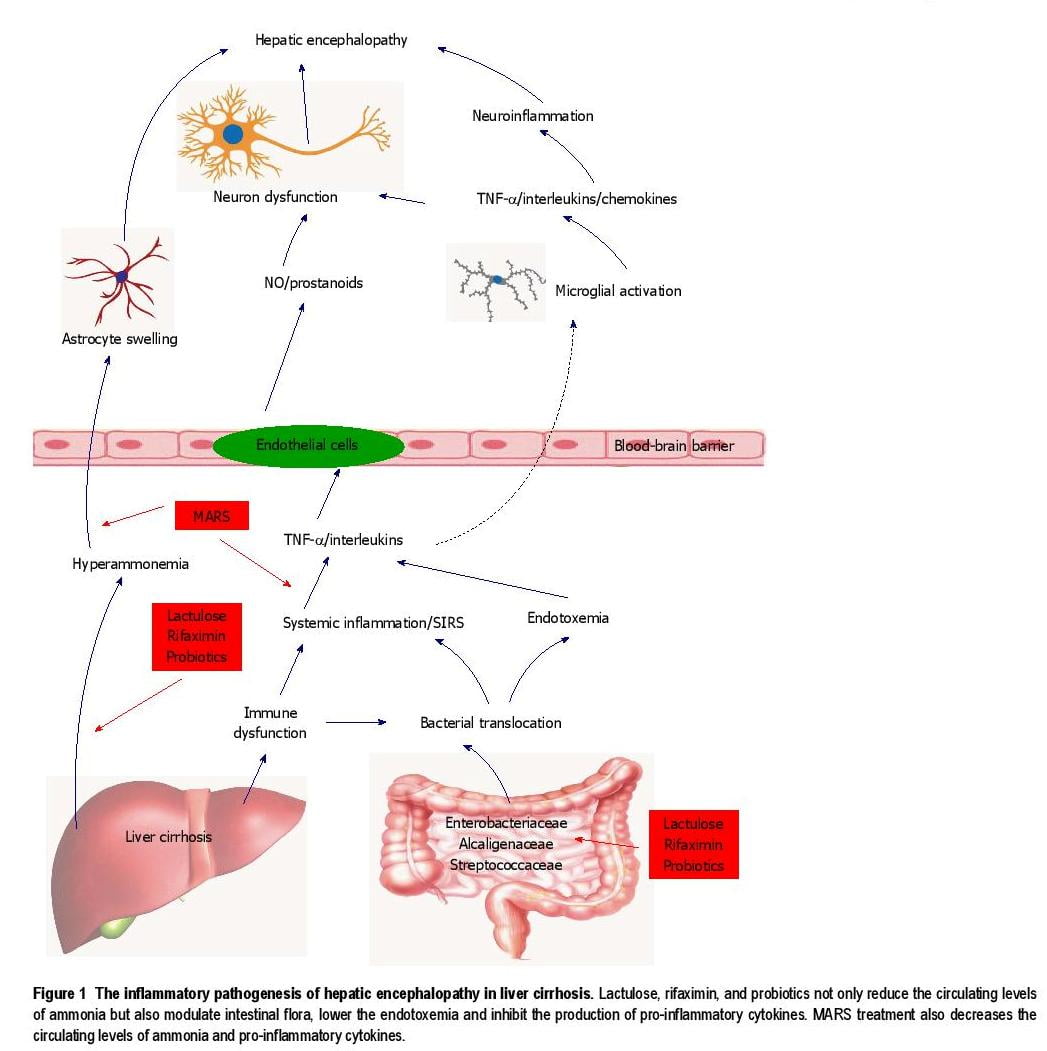
Over the past decade, increasing evidence has indicated that inflammation, including systemic inflammation, neuroinflammation and endotoxemia, plays an important role in the pathogenesis of HE, and inflammation is gradually being considered a critical therapeutic target for HE in cirrhotic patients[5,10,11]. Meanwhile, the current therapies for HE, such as lactulose, rifaximin, probiotics and the molecular adsorbent recirculating system (MARS), have been found to modulate the inflammatory response and lower pro-inflammatory mediator levels, which help to improve the clinical manifestations and delay the progression of HE in cirrhotic patients (Figure 1)[12-15]. These recent findings have demonstrated the possibility of these therapies in ameliorating inflammation and providing a novel and promising therapeutic alternative for patients with HE secondary to liver cirrhosis. This review summarizes the inflammatory mechanisms implicated in the pathogenesis of HE and evaluates the evidence of current therapies that target the inflammatory pathogenesis of HE in clinical practice.
INFLAMMATORY PATHOGENESIS OF HE IN CIRRHOSIS
Systemic inflammation
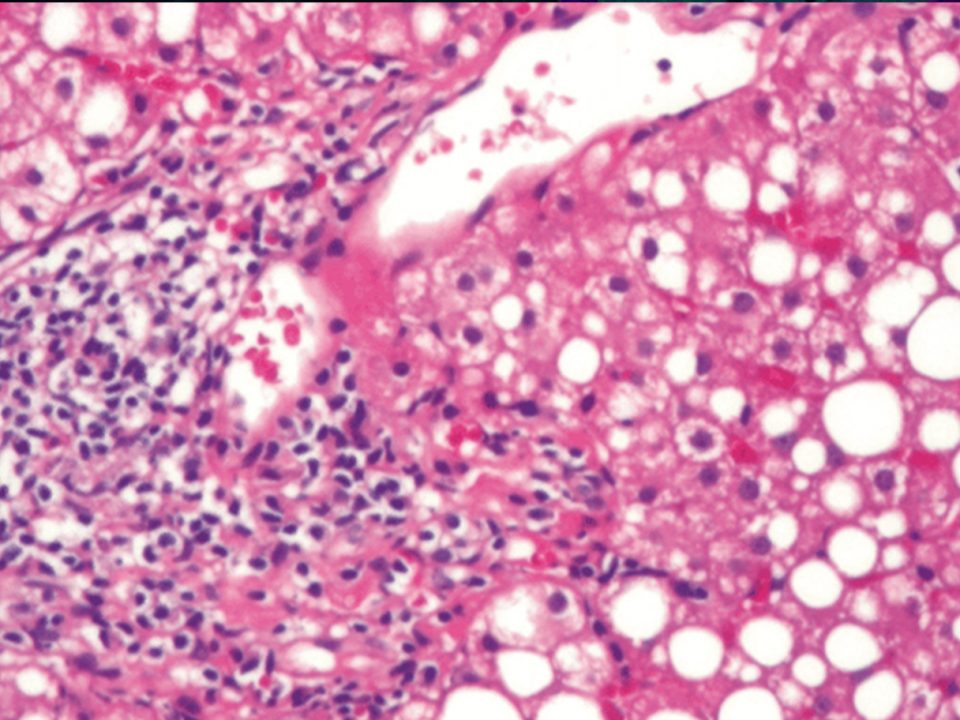
Cirrhotic patients are commonly found to have substantial disturbances of intestinal flora, with significant small intestinal overgrowth of potentially pathogenic Gram-negative bacteria, including Enterobacteriaceae, Alcaligenaceae and Streptococcaceae[16]. Furthermore, intestinal vascular congestion caused by portal hypertension, oxidative damage of the intestinal mucosa and the absence of mucosal immunoglobulin A secretion in cirrhosis have been demonstrated to result in increased intestinal permeability and intestinal barrier dysfunction[17]. Furthermore, ammonia induces neutrophil and macrophage dysfunction and impairs phagocytosis, which may culminate in a “sepsislike” immune paralysis[18,19]. These mechanisms synergistically induce the bacterial translocation that includes the migration of bacteria or bacterial byproducts from the small intestine to the systemic circulation, ultimately leading to spontaneous bacterial peritonitis and further systemic infection in patients with liver cirrhosis[20]. The study by Caly et al[21] has indicated that infection is the reason for hospital admission in 30% to 50% of cirrhotic patients, and 15% to 35% of them ultimately develop nosocomial infections during their hospital stay. Predominant infections presented in decompensated cirrhosis are spontaneous bacterial peritonitis, urinary tract infections, nosocomial pneumonia, sepsis and even systemic inflammatory response syndrome (SIRS)[22].
Circulating levels of pro-inflammatory cytokines, including tumor necrosis factor-α (TNF-α) and interleukins (ILs), are significantly elevated in decompensated cirrhotic patients[23]. These cytokines cannot exert their direct effects on the brain because they are unable to directly cross the blood-brain barrier (BBB). However, recent studies have demonstrated that TNF-α and IL-1β can influence the permeability of the BBB, and these peripheral cytokines exert their effects on the brain via the following three pathways: (1) peripheral tissues convey signals to the brain through the activation of the vagus nerve’s afferent neurons; (2) the brain vasculature sends signals through secondary messengers that are produced in response to cytokines, such as nitric oxide (NO) and prostanoids; and (3) cytokines enter brain areas that lack the BBB, and, subsequently, act at the brain parenchyma[24].
There is mounting clinical evidence for the role of systemic inflammation in the development of overt and minimal HE in cirrhotic patients. Serum concentrations of TNF-α and IL-6 have been found to correlate positively with the severity of overt HE in decompensated cirrhotic patients, and TNF-α is believed to be strongly involved in the pathogenesis of HE due
to chronic liver failure[25-27]. Furthermore, systemic infection/SIRS, but not ammonia, was correlated with increasing grades of overt HE in cirrhotic patients with grades Ⅲ–Ⅳ HE[5]. Similarly, serum levels of TNF-α, IL-6 and IL-18 were associated with the severity of minimal HE, and serum levels of IL-6 and IL-18 might have the capacity to identify cirrhotic patients with and without minimal HE[28,29]. In addition, Shawcross et al[6] have reported that the presence and severity of minimal HE were not correlated with ammonia concentrations, but serum levels of inflammatory markers, including C-reactive protein and IL-6, were significantly higher in cirrhotic patients with minimal HE compared with those without, which indicated that systemic inflammation is a critical determinant of the presence and severity of minimal HE.
Neuroinflammation
Neuroinflammation is considered to be an inflammatory response in the brain and is featured by microglial activation and the cerebral production of pro-inflammatory mediators[10]. Neuroinflammation is closely associated with systemic inflammation. Vascular endothelial cells, along with astrocytes, are a major constituent of the BBB. Endothelial cells induce the release of different pro-inflammatory mediators into the brain when they are stimulated by systemic inflammation[30]. For instance, endothelial cells have receptors for TNF-α and IL-1β, and these receptors convey signals that induce the synthesis of secondary messengers in the brain, such as NO and prostanoids[31]. Moreover, microglial cells constitute the resident macrophages of the brain and can be activated by proinflammatory mediators, releasing various types of chemokines with inflammatory properties[32]. These mechanisms have been demonstrated to contribute to the development of neuroinflammation in the brain.
Evidence for the role of neuroinflammation in the pathogenesis of HE due to cirrhosis has recently been provided by several animal experiments. Motor deficits, psychomotor slowing and hypokinesia are commonly presented in cirrhotic patients with HE, which can be simulated in rats with a portacaval shunt (PCS) and bile duct ligation (BDL), according to the recommendation by the International Society for Hepatic Encephalopathy and Nitrogen Metabolism (ISHEN)[33]. A study by Cauli et al[34] revealed that PCS rats exhibited increased levels of IL-6 and increased activities of cyclooxygenase and inducible NO synthase in the cerebral cortex, indicating the presence of neuroinflammation. Subsequently, chronic treatment with an anti-inflammatory drug, ibuprofen, could normalize the activities of cyclooxygenase and inducible NO synthase and completely restore the learning ability of PCS rats. In addition, BDL activated the microglia in the cerebellum, increased levels of inducible NO synthase, IL-1β and prostaglandin E2, and impaired the rats’ cognitive and motor functions. Similarly, ibuprofen also ameliorated neuroinflammation and restored the cognitive and motor functions of BDL rats[35]. These findings indicate that neuroinflammation contributes to cognitive and motor alterations in experimental animal models of HE and point to the possibility that the anti-inflammatory treatment may improve cognitive deficits in cirrhotic patients with HE. However, in cirrhotic patients with HE, microglial activation has not been found to be correlated with increased mRNA expression of TNF-a, IL-1β and IL-6 in the cerebral cortex[36]. Furthermore, compared with the controls, mRNA profiles of these cytokines remained unchanged in the brains of cirrhotic patients with HE, despite an up-regulation of genes associated with microglial activation[37]. The underlying reason responsible for this inconsistency is unclear; thus, further studies are required to clarify the role of neuroinflammation in the inflammatory pathogenesis of HE secondary to liver cirrhosis.
Endotoxemia
Due to intestinal bacterial translocation and portosystemic shunting, endotoxin, the lipopolysaccharide in the outer membrane of Gram-negative bacteria, enters the systemic circulation and is responsible for long-standing endotoxemia[17]. Endotoxin is able to activate immune cells either through activating Toll-like receptors or by inducing the production of pro-inflammatory cytokines[38]. Similar to pro-inflammatory cytokines, endotoxin also cannot cross the BBB, but it increases BBB permeability and acts on the brain parenchyma through endothelial cell receptor interactions with the downstream production of NO and prostanoid[39,40].
Henry et al[41] found that a peripheral lipopolysaccharide injection induced a hyperactive microglial activation in the brains of mice and resulted in a significant induction of mRNA expression of both IL1β and IL-10 in the cerebral cortex of aged mice. In addition, lipopolysaccharide that was injected into the rats’ hippocampus could lead to microglial activation and increased production of TNF-α and IL-1β in the hippocampus, inducing a reduction of glutamatergic transmission that led to learning and memory deficits without neuronal cell death[42]. Endotoxemia without sepsis has been reported in patients with liver cirrhosis and was found to be associated with an increased incidence of overt HE and mortality in these patients[43]. Moreover, a study by Jain et al[11] showed that serum levels of endotoxin were correlated with the severity of minimal HE due to cirrhosis. Endotoxemia may play a crucial role in the inflammatory pathogenesis of HE, especially in compensated cirrhotic patients without evidence of proven infection.
Ammonia-inflammation synergism
Decompensated cirrhosis results in both systemic inflammation and hyperammonemia. At the cellular level, TNF-α and IL-6 influence the permeability of the BBB, and human cerebrovascular endothelial cells increased ammonia uptake when exposed to TNF-α in vitro[44]. On the background of hyperammonemia, neuroinflammation involving both pro-inflammatory and neurotransmitter pathways can be induced by systemic inflammatory stimulus[45]. Furthermore, hyperammonemia leads to lactate accumulation in the brain, and both systemic inflammation and brain lactate accumulation lead to microglial activation and the increased production of TNF-α, IL-1β and IL-6[46]. Therefore, it is believed that ammonia potentially acts in concert with inflammation in a synergistic manner in the pathogenesis of HE.
Marini et al[47] found that mice with chronic hyperammonemia exhibited prolonged cognitive and motor deficits when treated with a lipopolysaccharide stimulus. Furthermore, chronic hyperammonemia has been found to induce microglial activation and subsequent neuroinflammation that were associated with the cognitive and motor deficits of BDL rats[35]. In a study by Jover et al[48], although both BDL and ammonia-fed BDL rats exhibited microglial activation in the brain, ammonia-fed BDL rats showed severe motor deficits compared to BDL rats, whose motor functions seemed only mildly influenced. Likewise, cirrhotic patients with systemic inflammation and hyperammonemia also showed significant impairments of cognitive and motor functions. For example, Shawcross et al[49] have reported that systemic infection/SIRS exacerbated the neuropsychological deterioration induced by hyperammonemia in cirrhotic patients with overt HE. Moreover, in cirrhotic patients with minimal HE, there were considerable cognitive impairments following induced hyperammonemia during infection, but not after its resolution[6]. In addition, Felipo et al[50] have found that hyperammonemia or inflammation alone did not result in cognitive impairments, but the synergistic effect of hyperammonemia and inflammation was sufficient to induce cognitive impairments in cirrhotic patients with minimal HE. This evidence suggests that, on the background of cirrhosis, inflammation and its mediators modulate the cerebral effect of hyperammonemia, and there is a synergistic relationship between hyperammonemia and inflammation in the pathogenesis of HE in liver cirrhosis.
CURRENT THERAPIES TARGETING THE INFLAMMATORY PATHOGENESIS OF HE
Non-absorbable disaccharides
Non-absorbable disaccharides, including lactulose and lactitol, lower the production and absorption of ammonia and are traditionally considered the current mainstay therapy for HE. Recently, emerging studies have indicated that non-absorbable disaccharides not only reduce circulating levels of ammonia but also decrease those of pro-inflammatory cytokines and endotoxin. For example, Jia et al[51] showed that lactulose lowered the level of hyper-endotoxemia, improved the cognitive and motor functions, and decreased the incidence of minimal HE in a rat model. Similarly, in cirrhotic patients with minimal HE, lactulose regulated the stool microbiome, lowered the level of serum endotoxin, inhibited the production of TNF-α, IL-2, IL-6 and IL-13, and consequently, improved their psychometric function[12]. Moreover, a study by Jain et al[11] revealed that lactulose inhibited intestinal bacterial overgrowth, significantly reduced the serum concentrations of TNF-α, IL-6, IL-18 and endotoxin, and subsequently improved cognitive functions in cirrhotic patients with minimal HE. By contrast, lactulose withdrawal resulted in a mixed inflammatory response and cognitive deterioration in cirrhotic patients with minimal HE[52]. In addition, lactulose improved cognitive and motor functions in cirrhotic patients with minimal HE, which helped to improve health-related quality of life, prevent motor vehicle accidents and reduce societal costs[3,53]. For cirrhotic patients with overt HE, a meta-analysis of randomized clinical trials showed that lactulose had beneficial effects on overt HE manifestations, and lactulose has been demonstrated to be efficacious in the secondary prevention of overt HE[54,55]. Given their cost and availability, non-absorbable disaccharides are likely to remain a well-used therapy in HE.
The side effects of non-absorbable disaccharide treatment include flatulence, diarrhea, abdominal pain and intestinal malabsorption, resulting in frequent noncompliance in cirrhotic patients with HE[56]. Additionally, despite substantial evidence of the beneficial effects of non-absorbable disaccharides, their efficacy and safety for HE have been recently questioned. For example, a Cochrane review revealed that clinical trials with high methodological quality found no significant effect of non-absorbable disaccharides on the risk of no improvement in HE and mortality[56]. Thus, there has been insufficient evidence to determine whether non-absorbable disaccharides are of benefit to cirrhotic patients with HE, and more high-quality studies are required in the future.
Rifaximin
Antibiotics are able to eliminate pathogenic Gramnegative bacteria in the intestinal tract, inhibit bacterial translocation, and consequently, decrease the overproduction of pro-inflammatory cytokines and endotoxin. Prominent antibiotics used in the treatment of HE are neomycin, metronidazole, vancomycin and rifaximin; however, extensive side-effect profiles and the potential for bacterial antimicrobial resistance have limited the utility of most of these antibiotics in treating HE, with the exception of rifaximin, which is the only systematically studied antibiotic and has substantial clinical evidence[57].
Rifaximin is a non-absorbable antibiotic with wide antimicrobial activity against both aerobic and anaerobic Gram-negative bacteria[58]. Recently, Vlachogiannakos et al[59] found that selective intestinal decontamination with a rifaximin regimen significantly ameliorated endotoxemia in patients with decompensated alcohol-related cirrhosis. Furthermore, the studies by Kalambokis et al[60,61] revealed that rifaximin could decrease serum concentrations of TNF-α, IL-6 and endotoxin in patients with alcoholic cirrhosis. In cirrhotic patients with minimal HE, rifaximin was found to alter intestinal bacterial linkages with metabolites without considerable changes in the intestinal flora, decrease the circulating levels of endotoxemia, and improve cognitive function[13]. These results indicate that rifaximin can regulate the intestinal flora, reduce the production of endotoxin and pro-inflammatory cytokines and ultimately improve cognitive function in cirrhotic patients with HE.
The clinical efficacy of rifaximin as a treatment for HE has been extensively explored in several clinical trials. For example, a prospective randomized, doubleblind, controlled trial found that rifaximin significantly improved mental state, electroencephalogram irregularities and portal-systemic encephalopathy index in cirrhotic patients with gradesⅠ-Ⅲ acute HE[62]. Compared with lactulose, treatment of HE with rifaximin was correlated with decreased hospitalization duration, lower hospitalization expenses and better clinical manifestations[63]. Moreover, a large, doubleblinded, randomized, controlled study by Bass et al[64] has demonstrated that rifaximin not only significantly reduced the risk of hospitalization involving HE but also effectively maintained remission from HE. In these clinical trials, rifaximin was well-tolerated, and fewer adverse events were reported compared with treatments with non-absorbable disaccharides. These results suggest that rifaximin may be an effective alternative treatment to non-absorbable disaccharides in treating HE, with an acceptable side effect profile.
As mentioned above, lactulose has no beneficial impact on the mortality of cirrhotic patients with HE. Different from lactulose, Sharma et al[65] have demonstrated that rifaximin significantly reduced the mortality of cirrhotic patients with HE, and the combination of lactulose plus rifaximin was more effective than lactulose alone in the treatment of HE. Furthermore, a systematic review with meta-analysis by Kimer et al[66] showed that rifaximin increased the proportion of patients whose neuropsychiatric manifestations improved and reduced mortality, which indicated that rifaximin should be used for secondary prevention of HE; however, although rifaximin did result in lower readmission rates for HE at half a year, the addition of rifaximin to lactulose for treating acute HE did not reduce hospital length of stay[67]. Therefore, the efficiency of combined treatment with lactulose plus rifaximin should be further evaluated by more randomized and controlled clinical trials. Probiotics Probiotics are living beneficial bacteria in the intestinal tract, and they are able to inhibit the activity of bacterial ureases, modulate intestinal pH values, and ultimately, reduce ammonia absorption[68]. Recently, probiotics have been reported to inhibit the bacterial activators of Toll-like receptors (TLRs), lower endogenous levels of IL-10 and TLR-4 expression, and ultimately, restore neutrophil phagocytic activity in alcohol-related cirrhotic patients[69]. Furthermore, probiotics modulate derangements in gut microbiota via inhibiting the overgrowth of pathogenic bacteria and prevent bacterial translocation, thus significantly lowering serum levels of endotoxin, which may help to inhibit the production and activity of pro-inflammatory cytokines[70].
The past decade has witnessed an upsurge of interest in the utility of probiotics for treating minimal HE in cirrhotic patients. For instance, in a phaseⅠclinical trial, the probiotic Lactobacillus GG reduced Enterobacteriaceae, increased the relative abundance of Clostridiales Incertae Sedis XIV and Lachnospiraceae, and further decreased endotoxemia and serum concentrations of TNF-α in cirrhotic patients with minimal HE, suggesting that Lactobacillus GG modulates intestinal dysbiosis and prevents systemic inflammatory response in these patients[14]. During this study, however, there was no significant improvement in cognitive functions before or after Lactobacillus GG treatment, and Lactobacillus GG was correlated with a markedly higher percent of self-limited diarrhea, which gives impetus to further studies regarding probiotics for treating minimal HE in cirrhotic patients. In addition, synbiotics (i.e., probiotics and fermentable fiber) treatment significantly increased the fecal content of the non-urease-producing Lactobacillus species at the expense of these other bacterial species, which was correlated with a marked decrease in endotoxemia and a reversal of minimal HE in 50% of cirrhotic patients[71]. Furthermore, a multi-strain probiotic compound containing Lactobacillus, Bifidobacterium strains and S. thermophiles improved the neuropsychological manifestations of cirrhotic patients with minimal HE, and these probiotics had longer-term therapeutic effects than lactulose[72]. Moreover, probiotic VSL#3 was found to be non-inferior to the standard therapy, lactulose, in treating minimal HE[73]. Nevertheless, a meta-analysis by Shukla et al[74] revealed that lactulose appeared to have the most beneficial effect in minimal HE, followed by probiotics and synbiotics. Probiotics may take the place of lactulose for the standard treatment of minimal HE, but this possibility should be evaluated by more controlled trials that compare their efficacy.
In the above-mentioned clinical trials, the side effects of probiotics were reported to be mild, and there have been no reported adverse events related to treatment with probiotics in minimal HE; however, a randomized, controlled trial by Besselink et al[75] revealed that probiotics did not reduce the risk of infectious complications, and they were correlated with an increased risk of mortality in patients with predicted severe acute pancreatitis. Similarly, whether oral supplementation with probiotics may induce infectious complications in cirrhotic patients with HE requires further investigation, especially in those with severe infection. Furthermore, an updated metaanalysis by Xu et al[76] found that although probiotics significantly prevented the development of HE, they did not affect serum ammonia levels or cirrhotic patients’ mortality. In addition, a Cochrane review by McGee et al[77] showed that there was no sufficient evidence of clinically significant improvement in HE treated with probiotics, and probiotics were especially shown to have no benefit to mortality. Therefore, the use of probiotics for cirrhotic patients with HE cannot be currently recommended, and rigorous clinical evaluation in randomized controlled trials is required.
MARS
Extracorporeal albumin dialysis, especially MARS, is a new method of hemodiafiltration in which blood is dialyzed against an albumin-containing solution across a high-flux membrane, which allows for the combined elimination of albumin-bound and water-soluble toxins. A Cochrane review by Liu et al[78] revealed that MARS treatment reduced the mortality of patients with acute-on-chronic liver failure (ACLF) and had a beneficial effect on HE. For example, Dominik et al[79] reported that treatment with MARS decreased the serum concentrations of TNF-α and IL-6 in patients with ACLF due to cirrhosis. In a study by Guo et al[15], MARS treatment significantly decreased serum levels of TNF-α, IL-6, IL-8 and INF-γ, which was associated with improvements of HE in ACLF. Furthermore, results of a study by Sen et al[80] showed that MARS treatment improved HE manifestations in patients with inflammation-related ACLF, and the main therapeutic effect of MARS was on other inflammatory mediators, such as NO, that were reduced by a combination of their elimination and decreased production. Taken together, these results suggest that MARS is regarded as a potentially effective alternative for eliminating inflammatory mediators from the circulation and ameliorating HE manifestations in ACLF patients who fail to respond to conventional therapy.
MARS has been demonstrated to be beneficial for HE secondary to ACLF; however, its efficacy did not appear to be associated with alterations in the serum levels of pro-inflammatory cytokines. In patients with ACLF, Stadlbauer et al[81] found that cytokines were eliminated from plasma by MARS treatment; however, MARS could not lower the serum cytokines levels. This difference may be attributed to increased cytokine production in ACLF. Furthermore, a prospective, multi-center trial by Hassanein et al[82] revealed that although MARS treatment improved grades Ⅲ and Ⅳ HE earlier than standard medical therapy in ACLF patients, there was no significant difference in SIRS scores between MARS treatment and standard medical therapy. Moreover, although the neurological manifestations of patients with HE were improved, no significant change in the serum concentrations of TNF-α, IL-6 and IL-8 was observed before vs after MARS treatment in ACLF, and MARS treatment did not exhibit a clearly identifiable efficacy in eliminating these circulating cytokines[83]. Although the above-mentioned clinical trials support the fact that MARS treatment is of benefit to the improvement of HE, these trials did not specifically evaluate the efficacy of MARS treatment in HE and were designed to only examine the improvements of ACLF. Therefore, the therapeutic effect of MARS treatment on the inflammatory pathogenesis of HE awaits the completion of further clinical trials.
CONCLUSION
HE is a serious neuropsychiatric complication of liver cirrhosis, and inflammation is a critical participating factor in the pathogenesis of HE. As mentioned above, existing therapies including lactulose, rifaximin, probiotics and MARS have been demonstrated to be beneficial for HE in cirrhotic patients by ameliorating the inflammatory pathogenesis of HE. These recent findings indicate that inflammation should be considered an important therapeutic target for HE and also point to the possibility that anti-inflammatory therapies will be promising alternatives for the treatment of HE in cirrhotic patients; however, the efficacy of these alternatives has not been fully confirmed and their safety is still questioned. Furthermore, the influence of these alternatives on the prognosis of cirrhotic patients with HE has remained controversial. Therefore, in the future, more multi-center, randomized, controlled trials are required to evaluate the efficacy and safety of these alternatives.
Conflict of interest: The authors have no conflicts of interest to declare in relation to this manuscript.
1 Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, Weissenborn K, Wong P. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology 2014; 60: 715-735 [PMID: 25042402 DOI: 10.1002/hep.27210]
2 Ortiz M, Jacas C, Córdoba J. Minimal hepatic encephalopathy: diagnosis, clinical significance and recommendations. J Hepatol 2005; 42 Suppl: S45-S53 [PMID: 15777572 DOI: 10.1016/j.jhep]
3 Prasad S, Dhiman RK, Duseja A, Chawla YK, Sharma A, Agarwal R. Lactulose improves cognitive functions and health-related quality of life in patients with cirrhosis who have minimal hepatic encephalopathy. Hepatology 2007; 45: 549-559 [PMID: 17326150 DOI: 10.1002/hep]
4 Bajaj JS, Saeian K, Verber MD, Hischke D, Hoffmann RG, Franco J, Varma RR, Rao SM. Inhibitory control test is a simple method to diagnose minimal hepatic encephalopathy and predict development of overt hepatic encephalopathy. Am J Gastroenterol 2007; 102: 754-760 [PMID: 17222319 DOI: 10.1111/j.1572-0241.2007.01048.x]
5 Castro-Tavares J. Effects of isoprenaline and phenylephrine on plasma potassium: role of the liver. Arch Int Pharmacodyn Ther 1975; 218: 110-119 [PMID: 2116 DOI: 10.1016/j.jhep.2010.07.045]
6 Shawcross DL, Wright G, Olde Damink SW, Jalan R. Role of ammonia and inflammation in minimal hepatic encephalopathy. Metab Brain Dis 2007; 22: 125-138 [PMID: 17260161 DOI: 10.1007/s11011-006-9042-1]
7 Ong JP, Aggarwal A, Krieger D, Easley KA, Karafa MT, Van Lente F, Arroliga AC, Mullen KD. Correlation between ammonia levels and the severity of hepatic encephalopathy. Am J Med 2003; 114: 188-193 [PMID: 12637132 DOI: 10.1016/S0002-9343(02)01477-8]
8 Sharma P, Sharma BC, Sarin SK. Predictors of nonresponse to lactulose in patients with cirrhosis and hepatic encephalopathy. Eur J Gastroenterol Hepatol 2010; 22: 526-531 [PMID: 20009938 DOI: 10.1097/MEG.0b013e3283341b7d]
9 Als-Nielsen B, Gluud LL, Gluud C. Non-absorbable disaccharides for hepatic encephalopathy: systematic review of randomised trials. BMJ 2004; 328: 1046 [PMID: 15054035]
10 Butterworth RF. The liver-brain axis in liver failure: neuroinflammation and encephalopathy. Nat Rev Gastroenterol Hepatol 2013; 10: 522-528 [PMID: 23817325 DOI: 10.1038/nrgastro]
11 Jain L, Sharma BC, Srivastava S, Puri SK, Sharma P, Sarin S. Serum endotoxin, inflammatory mediators, and magnetic resonance spectroscopy before and after treatment in patients with minimal hepatic encephalopathy. J Gastroenterol Hepatol 2013; 28: 1187-1193 [PMID: 23425082 DOI: 10.1111/jgh.12160]
12 Bajaj JS, Ridlon JM, Hylemon PB, Thacker LR, Heuman DM, Smith S, Sikaroodi M, Gillevet PM. Linkage of gut microbiome with cognition in hepatic encephalopathy. Am J Physiol Gastrointest Liver Physiol 2012; 302: G168-G175 [PMID: 21940902 DOI: 10.1152/ ajpgi.00190]
13 Bajaj JS, Heuman DM, Sanyal AJ, Hylemon PB, Sterling RK, Stravitz RT, Fuchs M, Ridlon JM, Daita K, Monteith P, Noble NA, White MB, Fisher A, Sikaroodi M, Rangwala H, Gillevet PM. Modulation of the metabiome by rifaximin in patients with cirrhosis and minimal hepatic encephalopathy. PLoS One 2013; 8: e60042 [PMID: 23565181 DOI: 10.1371/journal.pone]
14 Bajaj JS, Heuman DM, Hylemon PB, Sanyal AJ, Puri P, Sterling RK, Luketic V, Stravitz RT, Siddiqui MS, Fuchs M, Thacker LR, Wade JB, Daita K, Sistrun S, White MB, Noble NA, Thorpe C, Kakiyama G, Pandak WM, Sikaroodi M, Gillevet PM. Randomised clinical trial: Lactobacillus GG modulates gut microbiome, metabolome and endotoxemia in patients with cirrhosis. Aliment Pharmacol Ther 2014; 39: 1113-1125 [PMID: 24628464 DOI: 10.1111/apt.12695]
15 Guo LM, Liu JY, Xu DZ, Li BS, Han H, Wang LH, Zhang WY, Lu LH, Guo X, Sun FX, Zhang HY, Liu XD, Zhang JP, Yao Y, He ZP, Wang MM. Application of Molecular Adsorbents Recirculating System to remove NO and cytokines in severe liver failure patients with multiple organ dysfunction syndrome. Liver Int 2003; 23 Suppl 3: 16-20 [PMID: 12950956 DOI: 10.1034/j.1478]
16 Garcovich M, Zocco MA, Roccarina D, Ponziani FR, Gasbarrini A. Prevention and treatment of hepatic encephalopathy: focusing on gut microbiota. World J Gastroenterol 2012; 18: 6693-6700 [PMID: 23239905 DOI: 10.3748/wjg.v18.i46.6693]
17 Bellot P, Francés R, Such J. Pathological bacterial translocation in cirrhosis: pathophysiology, diagnosis and clinical implications. Liver Int 2013; 33: 31-39 [PMID: 23121656]
18 Shawcross DL, Wright GA, Stadlbauer V, Hodges SJ, Davies NA, Wheeler-Jones C, Pitsillides AA, Jalan R. Ammonia impairs neutrophil phagocytic function in liver disease. Hepatology 2008; 48: 1202-1212 [PMID: 18697192 DOI: 10.1002/hep.22474]
19 Wasmuth HE, Kunz D, Yagmur E, Timmer-Stranghöner A, Vidacek D, Siewert E, Bach J, Geier A, Purucker EA, Gressner AM, Matern S, Lammert F. Patients with acute on chronic liver failure display “sepsis-like” immune paralysis. J Hepatol 2005; 42: 195-201 [PMID: 15664244 DOI: 10.1016/j.jhep.2004.10.019]
20 Wiest R, Lawson M, Geuking M. Pathological bacterial translocation in liver cirrhosis. J Hepatol 2014; 60: 197-209 [PMID: 23993913 DOI: 10.1016/j.jhep.2013.07.044]
21 Caly WR, Strauss E. A prospective study of bacterial infections in patients with cirrhosis. J Hepatol 1993; 18: 353-358 [PMID: 8228129]
22 Fernández J, Navasa M, Gómez J, Colmenero J, Vila J, Arroyo V, Rodés J. Bacterial infections in cirrhosis: epidemiological changes with invasive procedures and norfloxacin prophylaxis. Hepatology 2002; 35: 140-148 [PMID: 11786970 DOI: 10.1053/ jhep.2002.30082]
23 Tilg H, Wilmer A, Vogel W, Herold M, Nölchen B, Judmaier G, Huber C. Serum levels of cytokines in chronic liver diseases. Gastroenterology 1992; 103: 264-274 [PMID: 1612333]
24 Licinio J, Wong ML. Pathways and mechanisms for cytokine signaling of the central nervous system. J Clin Invest 1997; 100: 2941-2947 [PMID: 9399938 DOI: 10.1172/JCI119846]
25 Odeh M, Sabo E, Srugo I, Oliven A. Serum levels of tumor necrosis factor-alpha correlate with severity of hepatic encephalopathy due to chronic liver failure. Liver Int 2004; 24: 110-116 [PMID: 15078474 DOI: 10.1111/j.1478-3231.2004.0894.x]
26 Jain L, Sharma BC, Sharma P, Srivastava S, Agrawal A, Sarin SK. Serum endotoxin and inflammatory mediators in patients with cirrhosis and hepatic encephalopathy. Dig Liver Dis 2012; 44: 1027-1031 [PMID: 22883217 DOI: 10.1016/j.dld.2012.07.002]
27 Odeh M. Pathogenesis of hepatic encephalopathy: the tumour necrosis factor-alpha theory. Eur J Clin Invest 2007; 37: 291-304 [PMID: 17373965 DOI: 10.1111/j.1365-2362.2007.01778.x]
28 Montoliu C, Piedrafita B, Serra MA, del Olmo JA, Urios A, Rodrigo JM, Felipo V. IL-6 and IL-18 in blood may discriminate cirrhotic patients with and without minimal hepatic encephalopathy. J Clin Gastroenterol 2009; 43: 272-279 [PMID: 18562979 DOI: 10.1097/ MCG.0b013]
29 Luo M, Li L, Yang EN, Cao WK. Relationship between interleukin-6 and ammonia in patients with minimal hepatic encephalopathy due to liver cirrhosis. Hepatol Res 2012; 42: 1202-1210 [PMID: 22646055 DOI: 10.1111/j.1872-034X.2012.01047.x]
30 Saper CB. The dance of the perivascular and endothelial cells: mechanisms of brain response to immune signaling. Neuron 2010; 65: 4-6 [PMID: 20152108 DOI: 10.1016/j.neuron.2009.12.029]
31 Schiltz JC, Sawchenko PE. Signaling the brain in systemic inflammation: the role of perivascular cells. Front Biosci 2003; 8: s1321-s1329 [PMID: 12957837]
32 Hinkerohe D, Smikalla D, Haghikia A, Heupel K, Haase CG, Dermietzel R, Faustmann PM. Effects of cytokines on microglial phenotypes and astroglial coupling in an inflammatory coculture model. Glia 2005; 52: 85-97 [PMID: 15920725 DOI: 10.1002/ glia.20223]
33 Butterworth RF, Norenberg MD, Felipo V, Ferenci P, Albrecht J, Blei AT. Experimental models of hepatic encephalopathy: ISHEN guidelines. Liver Int 2009; 29: 783-788 [PMID: 19638106 DOI: 10.1111/j.1478-3231.2009.02034.x]
34 Cauli O, Rodrigo R, Piedrafita B, Boix J, Felipo V. Inflammation and hepatic encephalopathy: ibuprofen restores learning ability in rats with portacaval shunts. Hepatology 2007; 46: 514-519 [PMID: 17659565 DOI: 10.1002/hep.21734]
35 Rodrigo R, Cauli O, Gomez-Pinedo U, Agusti A, HernandezRabaza V, Garcia-Verdugo JM, Felipo V. Hyperammonemia induces neuroinflammation that contributes to cognitive impairment in rats with hepatic encephalopathy. Gastroenterology 2010; 139: 675-684 [PMID: 20303348 DOI: 10.1053/j.gastro.2010.03.040]
36 Zemtsova I, Görg B, Keitel V, Bidmon HJ, Schrör K, Häussinger D. Microglia activation in hepatic encephalopathy in rats and humans. Hepatology 2011; 54: 204-215 [PMID: 21452284 DOI: 10.1002/ hep.24326]
37 Görg B, Bidmon HJ, Häussinger D. Gene expression profiling in the cerebral cortex of patients with cirrhosis with and without hepatic encephalopathy. Hepatology 2013; 57: 2436-2447 [PMID: 23325665 DOI: 10.1002/hep.26265]
38 Manigold T, Böcker U, Hanck C, Gundt J, Traber P, Antoni C, Rossol S. Differential expression of toll-like receptors 2 and 4 in patients with liver cirrhosis. Eur J Gastroenterol Hepatol 2003; 15: 275-282 [PMID: 12610323 DOI: 10.1097/01. meg.0000050010.68425.cb]
39 Wong D, Dorovini-Zis K, Vincent SR. Cytokines, nitric oxide, and cGMP modulate the permeability of an in vitro model of the human blood-brain barrier. Exp Neurol 2004; 190: 446-455 [PMID: 15530883 DOI: 10.1016/j.expneurol.2004.08.008]
40 Chastre A, Bélanger M, Nguyen BN, Butterworth RF. Lipopolysaccharide precipitates hepatic encephalopathy and increases blood-brain barrier permeability in mice with acute liver failure. Liver Int 2014; 34: 353-361 [PMID: 23910048 DOI: 10.1111/ liv.12252]
41 Henry CJ, Huang Y, Wynne AM, Godbout JP. Peripheral lipopolysaccharide (LPS) challenge promotes microglial hyperactivity in aged mice that is associated with exaggerated induction of both pro-inflammatory IL-1beta and anti-inflammatory IL-10 cytokines. Brain Behav Immun 2009; 23: 309-317 [PMID: 18814846 DOI: 10.1016/j.bbi.2008.09.002]
42 Tanaka S, Ide M, Shibutani T, Ohtaki H, Numazawa S, Shioda S, Yoshida T. Lipopolysaccharide-induced microglial activation induces learning and memory deficits without neuronal cell death in rats. J Neurosci Res 2006; 83: 557-566 [PMID: 16429444]
43 Bigatello LM, Broitman SA, Fattori L, Di Paoli M, Pontello M, Bevilacqua G, Nespoli A. Endotoxemia, encephalopathy, and mortality in cirrhotic patients. Am J Gastroenterol 1987; 82: 11-15 [PMID: 3799574]
44 Duchini A, Govindarajan S, Santucci M, Zampi G, Hofman FM. Effects of tumor necrosis factor-alpha and interleukin-6 on fluid-phase permeability and ammonia diffusion in CNS-derived endothelial cells. J Investig Med 1996; 44: 474-482 [PMID: 8952229]
45 Shawcross DL, Shabbir SS, Taylor NJ, Hughes RD. Ammonia and the neutrophil in the pathogenesis of hepatic encephalopathy in cirrhosis. Hepatology 2010; 51: 1062-1069 [PMID: 19890967 DOI: 10.1002/hep.23367]
46 Andersson AK, Rönnbäck L, Hansson E. Lactate induces tumour necrosis factor-alpha, interleukin-6 and interleukin-1beta release in microglial- and astroglial-enriched primary cultures. J Neurochem 2005; 93: 1327-1333 [PMID: 15934951 DOI: 10.1111/ j.1471-4159.2005.03132.x]
47 Marini JC, Broussard SR. Hyperammonemia increases sensitivity to LPS. Mol Genet Metab 2006; 88: 131-137 [PMID: 16497529 DOI: 10.1016/j.ymgme.2005.12.013]
48 Jover R, Rodrigo R, Felipo V, Insausti R, Sáez-Valero J, GarcíaAyllón MS, Suárez I, Candela A, Compañ A, Esteban A, Cauli O, Ausó E, Rodríguez E, Gutiérrez A, Girona E, Erceg S, Berbel P, Pérez-Mateo M. Brain edema and inflammatory activation in bile duct ligated rats with diet-induced hyperammonemia: A model of hepatic encephalopathy in cirrhosis. Hepatology 2006; 43: 1257-1266 [PMID: 16729306 DOI: 10.1002/hep.21180]
49 Shawcross DL, Davies NA, Williams R, Jalan R. Systemic inflammatory response exacerbates the neuropsychological effects of induced hyperammonemia in cirrhosis. J Hepatol 2004; 40: 247-254 [PMID: 14739095 DOI: 10.1016/j.jhep.2003.10.016]
50 Felipo V, Urios A, Montesinos E, Molina I, Garcia-Torres ML, Civera M, Olmo JA, Ortega J, Martinez-Valls J, Serra MA, Cassinello N, Wassel A, Jordá E, Montoliu C. Contribution of hyperammonemia and inflammatory factors to cognitive impairment in minimal hepatic encephalopathy. Metab Brain Dis 2012; 27: 51-58 [PMID: 22072427 DOI: 10.1007/s11011-011]
51 Jia L, Zhang MH. Comparison of probiotics and lactulose in the treatment of minimal hepatic encephalopathy in rats. World J Gastroenterol 2005; 11: 908-911 [PMID: 15682492 DOI: 10.3748/ wjg.v11.i6.908]
52 Bajaj JS, Gillevet PM, Patel NR, Ahluwalia V, Ridlon JM, Kettenmann B, Schubert CM, Sikaroodi M, Heuman DM, Crossey MM, Bell DE, Hylemon PB, Fatouros PP, Taylor-Robinson SD. A longitudinal systems biology analysis of lactulose withdrawal in hepatic encephalopathy. Metab Brain Dis 2012; 27: 205-215 [PMID: 22527995 DOI: 10.1007/s11011-012-9303-0]
53 Bajaj JS, Pinkerton SD, Sanyal AJ, Heuman DM. Diagnosis and treatment of minimal hepatic encephalopathy to prevent motor vehicle accidents: a cost-effectiveness analysis. Hepatology 2012; 55: 1164-1171 [PMID: 22135042 DOI: 10.1002/hep.25507]
54 Gluud LL, Dam G, Borre M, Les I, Cordoba J, Marchesini G, Aagaard NK, Vilstrup H. Lactulose, rifaximin or branched chain amino acids for hepatic encephalopathy: what is the evidence? Metab Brain Dis 2013; 28: 221-225 [PMID: 23275147 DOI: 10.1007/s11011-012-9372-0]
55 Sharma BC, Sharma P, Agrawal A, Sarin SK. Secondary prophylaxis of hepatic encephalopathy: an open-label randomized controlled trial of lactulose versus placebo. Gastroenterology 2009; 137: 885-91, 891.e1 [PMID: 19501587 DOI: 10.1053/j.gastro.2009]
56 Als-Nielsen B, Gluud LL, Gluud C. Nonabsorbable disaccharides for hepatic encephalopathy. Cochrane Database Syst Rev 2004; (2): CD003044 [PMID: 15106187 DOI: 10.1002/14651858]
57 Patidar KR, Bajaj JS. Antibiotics for the treatment of hepatic encephalopathy. Metab Brain Dis 2013; 28: 307-312 [PMID: 23389621 DOI: 10.1007/s11011-013-9383-5]
58 Scarpignato C, Pelosini I. Experimental and clinical pharmacology of rifaximin, a gastrointestinal selective antibiotic. Digestion 2006; 73 Suppl 1: 13-27 [PMID: 16498249]
59 Vlachogiannakos J, Saveriadis AS, Viazis N, Theodoropoulos I, Foudoulis K, Manolakopoulos S, Raptis S, Karamanolis DG. Intestinal decontamination improves liver haemodynamics in patients with alcohol-related decompensated cirrhosis. Aliment Pharmacol Ther 2009; 29: 992-999 [PMID: 19210289 DOI: 10.1111/j.1365-2036.2009.03958.x]
60 Kalambokis GN, Mouzaki A, Rodi M, Pappas K, Fotopoulos A, Xourgia X, Tsianos EV. Rifaximin improves systemic hemodynamics and renal function in patients with alcohol-related cirrhosis and ascites. Clin Gastroenterol Hepatol 2012; 10: 815-818 [PMID: 22391344 DOI: 10.1016/j.cgh.2012.02.025]
61 Kalambokis GN, Mouzaki A, Rodi M, Tsianos EV. Rifaximin improves thrombocytopenia in patients with alcoholic cirrhosis in association with reduction of endotoxaemia. Liver Int 2012; 32: 467-475 [PMID: 22098272 DOI: 10.1111/j.1478-3231.2011.02650. x]
62 Mas A, Rodés J, Sunyer L, Rodrigo L, Planas R, Vargas V, Castells L, Rodríguez-Martínez D, Fernández-Rodríguez C, Coll I, Pardo A. Comparison of rifaximin and lactitol in the treatment of acute hepatic encephalopathy: results of a randomized, double-blind, doubledummy, controlled clinical trial. J Hepatol 2003; 38: 51-58 [PMID: 12480560 DOI: 10.1016/S0168-8278]
63 Leevy CB, Phillips JA. Hospitalizations during the use of rifaximin versus lactulose for the treatment of hepatic encephalopathy. Dig Dis Sci 2007; 52: 737-741 [PMID: 17245628 DOI: 10.1007/ s10620-006-9442-4]
64 Bass NM, Mullen KD, Sanyal A, Poordad F, Neff G, Leevy CB, Sigal S, Sheikh MY, Beavers K, Frederick T, Teperman L, Hillebrand D, Huang S, Merchant K, Shaw A, Bortey E, Forbes WP. Rifaximin treatment in hepatic encephalopathy. N Engl J Med 2010; 362: 1071-1081 [PMID: 20335583 DOI: 10.1056/NEJMoa0907893]
65 Sharma BC, Sharma P, Lunia MK, Srivastava S, Goyal R, Sarin SK. A randomized, double-blind, controlled trial comparing rifaximin plus lactulose with lactulose alone in treatment of overt hepatic encephalopathy. Am J Gastroenterol 2013; 108: 1458-1463 [PMID: 23877348 DOI: 10.1038/ajg.2013.219]
66 Kimer N, Krag A, Møller S, Bendtsen F, Gluud LL. Systematic review with meta-analysis: the effects of rifaximin in hepatic encephalopathy. Aliment Pharmacol Ther 2014; 40: 123-132 [PMID: 24849268 DOI: 10.1111/apt.12803]
67 Courson A, Jones GM, Twilla JD. Treatment of Acute Hepatic Encephalopathy: Comparing the Effects of Adding Rifaximin to Lactulose on Patient Outcomes. J Pharm Pract 2015; Epub ahead of print [PMID: 25586470 DOI: 10.1177/0897190014566312]
68 Cesaro C, Tiso A, Del Prete A, Cariello R, Tuccillo C, Cotticelli G, Del Vecchio Blanco C, Loguercio C. Gut microbiota and probiotics in chronic liver diseases. Dig Liver Dis 2011; 43: 431-438 [PMID: 21163715 DOI: 10.1016/j.dld.2010.10.015]
69 Stadlbauer V, Mookerjee RP, Hodges S, Wright GA, Davies NA, Jalan R. Effect of probiotic treatment on deranged neutrophil function and cytokine responses in patients with compensated alcoholic cirrhosis. J Hepatol 2008; 48: 945-951 [PMID: 18433921 DOI: 10.1016/j.jhep.2008]
70 Albillos A, de la Hera A. Multifactorial gut barrier failure in cirrhosis and bacterial translocation: working out the role of probiotics and antioxidants. J Hepatol 2002; 37: 523-526 [PMID: 12217607 DOI: 10.1016/S0168-8278(02)00265-9]
71 Liu Q, Duan ZP, Ha DK, Bengmark S, Kurtovic J, Riordan SM. Synbiotic modulation of gut flora: effect on minimal hepatic encephalopathy in patients with cirrhosis. Hepatology 2004; 39: 1441-1449 [PMID: 15122774 DOI: 10.1002/hep.20194]
72 Shavakhi A, Hashemi H, Tabesh E, Derakhshan Z, Farzamnia S, Meshkinfar S, Shavakhi S, Minakari M, Gholamrezaei A. Multistrain probiotic and lactulose in the treatment of minimal hepatic encephalopathy. J Res Med Sci 2014; 19: 703-708 [PMID: 25422653]
73 Pratap Mouli V, Benjamin J, Bhushan Singh M, Mani K, Garg SK, Saraya A, Joshi YK. Effect of probiotic VSL#3 in the treatment of minimal hepatic encephalopathy: A non-inferiority randomized controlled trial. Hepatol Res 2015; 45: 880-889 [PMID: 25266207 DOI: 10.1111/hepr.12429]
74 Shukla S, Shukla A, Mehboob S, Guha S. Meta-analysis: the effects of gut flora modulation using prebiotics, probiotics and synbiotics on minimal hepatic encephalopathy. Aliment Pharmacol Ther 2011; 33: 662-671 [PMID: 21251030 DOI: 10.1111/j.1365-2036.2010.04574]
75 Besselink MG, van Santvoort HC, Buskens E, Boermeester MA, van Goor H, Timmerman HM, Nieuwenhuijs VB, Bollen TL, van Ramshorst B, Witteman BJ, Rosman C, Ploeg RJ, Brink MA, Schaapherder AF, Dejong CH, Wahab PJ, van Laarhoven CJ, van der Harst E, van Eijck CH, Cuesta MA, Akkermans LM, Gooszen HG. Probiotic prophylaxis in predicted severe acute pancreatitis: a randomised, double-blind, placebo-controlled trial. Lancet 2008; 371: 651-659 [PMID: 18279948 DOI: 10.1016/S0140- 6736(08)60207-X]
76 Xu J, Ma R, Chen LF, Zhao LJ, Chen K, Zhang RB. Effects of probiotic therapy on hepatic encephalopathy in patients with liver cirrhosis: an updated meta-analysis of six randomized controlled trials. Hepatobiliary Pancreat Dis Int 2014; 13: 354-360 [PMID: 25100119]
77 McGee RG, Bakens A, Wiley K, Riordan SM, Webster AC. Probiotics for patients with hepatic encephalopathy. Cochrane Database Syst Rev 2011; (11): CD008716 [PMID: 22071855 DOI: 10.1002/14651858.CD008716.pub2]
78 Liu JP, Gluud LL, Als-Nielsen B, Gluud C. Artificial and bioartificial support systems for liver failure. Cochrane Database Syst Rev 2004; (1): CD003628 [PMID: 14974025 DOI: 10.1002/14651]
79 Dominik A, Stange J, Pfensig C, Borufka L, Weiss-Reining H, Eggert M. Reduction of elevated cytokine levels in acute/acuteon-chronic liver failure using super-large pore albumin dialysis treatment: an in vitro study. Ther Apher Dial 2014; 18: 347-352 [PMID: 24215331 DOI: 10.1111/1744-9987.12146]
80 Sen S, Davies NA, Mookerjee RP, Cheshire LM, Hodges SJ, Williams R, Jalan R. Pathophysiological effects of albumin dialysis in acute-on-chronic liver failure: a randomized controlled study. Liver Transpl 2004; 10: 1109-1119 [PMID: 15350001 DOI: 10.1002/ lt.20236]
81 Stadlbauer V, Krisper P, Aigner R, Haditsch B, Jung A, Lackner C, Stauber RE. Effect of extracorporeal liver support by MARS and Prometheus on serum cytokines in acute-on-chronic liver failure. Crit Care 2006; 10: R169 [PMID: 17156425 DOI: 10.1186/cc5119]
82 Hassanein TI, Tofteng F, Brown RS, McGuire B, Lynch P, Mehta R, Larsen FS, Gornbein J, Stange J, Blei AT. Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis. Hepatology 2007; 46: 1853-1862 [PMID: 17975845 DOI: 10.1002/hep.21930]
83 Ilonen I, Koivusalo AM, Höckerstedt K, Isoniemi H. Albumin dialysis has no clear effect on cytokine levels in patients with lifethreatening liver insufficiency. Transplant Proc 2006; 38: 3540-3543 [PMID: 17175326 DOI: 10.1016/j.transproceed.2006.10.058]